Cancer is a life-changing experience that can be challenging. Cancer survivors deserve the best support and care to restore their confidence and enhance their quality of life.
This article will discuss the various options available for breast augmentation for cancer survivors. We will explore the benefits and drawbacks of each technique and provide comprehensive information to empower you in making the best decision for your breast reconstruction journey.
Breast Augmentation for Cancer Survivors: Exploring Reconstruction Options
Breast augmentation for cancer survivors encompasses a variety of reconstruction techniques tailored to individual needs. It’s a pivotal step in the healing journey, offering physical restoration and psychological benefits. Here’s a concise overview of the options:
A Breast Augmentation Surgeon is a doctor who helps people change the size or shape of their chest to make them feel more confident. they perform surgeries to make the bust area larger or smaller.
Book A Consultation With Dr Tarek Bayazid
Top-rated Plastic Surgeon For Breast Augmentation in Dubai
Installment Plan Available
Types of Breast Reconstruction Options
Breast reconstruction options can be broadly categorized into three types:
Each approach has benefits and drawbacks depending on your unique situation, physical condition, and medical background. The following section will discuss these options in detail.
Implant-Based Reconstruction Option
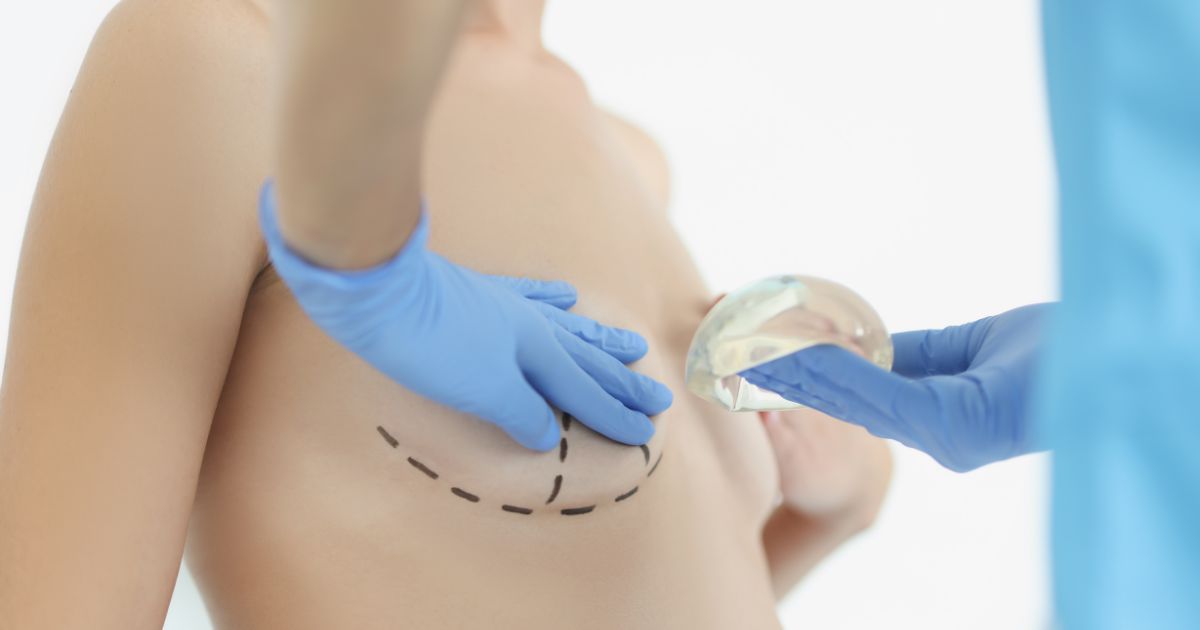
Implant-based reconstruction involves using saline or silicone breast implants to rebuild the breast shape. This method can be performed in two stages: tissue expander and implant placement.
Pros
Cons
Autologous Tissue Reconstruction
Autologous tissue reconstruction uses body tissue, such as skin, fat, and muscle, to reconstruct the breast. There are several techniques for this type of reconstruction, including:
Pros
Cons
Combination Reconstruction
Combination reconstruction combines the use of breast implants with autologous tissue techniques. This method can provide additional support and coverage for the implant, resulting in a more natural appearance and feel.
Pros
Cons
Nipple and Areola Reconstruction
After the breast mound is reconstructed, nipple and areola reconstruction can be performed to restore a more natural appearance. There are several methods for nipple and areola reconstruction, including:
Pros
Cons
Timing of Breast Reconstruction
Breast reconstruction can be performed at various times during the cancer treatment process:
The ideal timing for breast reconstruction depends on several factors, including your overall health, the stage of your cancer, and the recommended course of treatment. Discover Radiance at Dubai’s Top Aesthetic Clinic and experience the best beauty treatments that will make you shine. It’s like a magic place where they help you look your best! 300cc breast implants are used to make breasts look bigger and fuller they are a popular choice for people wanting a noticeable change.
What Factors to Consider for Breast Augmentation for Cancer Survivors?
The following elements should be taken into account while choosing your optimal breast reconstruction option:
To determine the best course of action for your unique situation, it is essential to have open and honest conversations with your healthcare team and plastic surgeon.
Breast reconstruction can be an empowering choice for cancer survivors, helping to restore a sense of normalcy and confidence by understanding the various options available, including implant-based, autologous tissue, and combination reconstruction.
Consider factors such as your overall health, cancer stage, and personal preferences when deciding on the best breast reconstruction option.
Are you prepared for the following stage in your breast reconstruction journey?
Request a quote from our experienced and compassionate team at Dr. Tarek Aesthetics. We are committed to providing personalised attention and help throughout the process, ensuring your best possible result.